Abstract
Obesity is a common comorbidity among patients with heart failure with reduced ejection fraction (HFrEF) or heart failure with preserved ejection fraction (HFpEF), with the strongest pathophysiologic link of obesity being seen for HFpEF. Lifestyle measures are the cornerstone of weight loss management, but sustainability is a challenge, and there are limited efficacy data in the heart failure (HF) population. Bariatric surgery has moderate efficacy and safety data for patients with preoperative HF or left ventricular dysfunction and has been associated with reductions in HF hospitalizations and medium-term mortality. Antiobesity medications historically carried concerns for cardiovascular adverse effects, but the safety and weight loss efficacy seen in general population trials of glucagon-like peptide 1 (GLP-1) and gastric inhibitory polypeptide/GLP-1 agonists are highly encouraging. Although there are safety concerns regarding GLP-1 agonists in advanced HFrEF, trials of the GLP-1 agonist semaglutide for treatment of obesity have confirmed safety and efficacy in patients with HFpEF.
Introduction
Heart failure (HF) remains a major public health challenge, imposing significant functional and quality of life (QoL) restrictions, economic burdens and persistently high rates of hospitalization and mortality.[1] The management of obesity and HF interlinks on multiple levels. Obesity is a potential contributor to HF development and may also exacerbate symptoms, functional limitations, and hospitalization rates for adults with established HF. The presence of obesity can furthermore complicate HF treatment options, especially for patients with advanced heart failure with reduced ejection fraction (HFrEF) in whom heart transplantation (HT) is being considered, and the presence of HF often affects the safety profile of medical and surgical therapeutic options for obesity.[2]
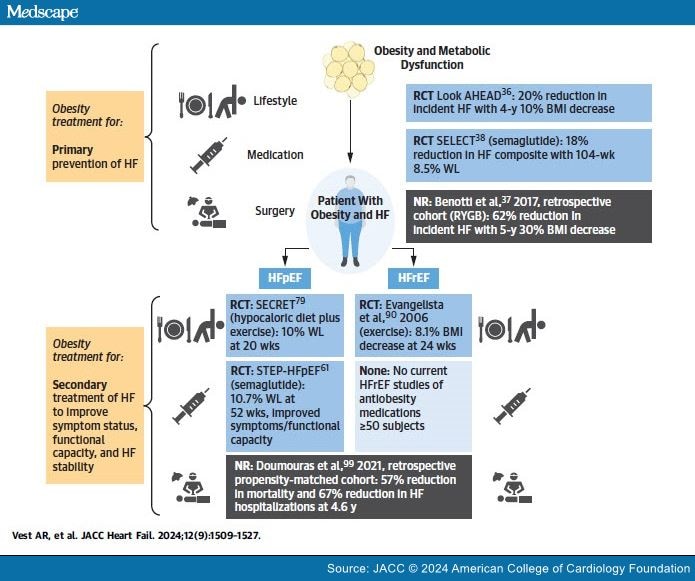
Historically, the presence of NYHA functional class II-IV HF has significantly limited opportunities to treat obesity across the lifestyle, metabolic and bariatric surgery (BSx), and pharmacologic domains of care. For example, earlier generations of pharmacotherapies approved for the treatment of obesity included stimulant medications with poor safety profiles for patients with HF. However, recent progress with the efficacy and safety of antiobesity medications (AOMs), as well as evolving experience with BSx in medically comorbid patient populations, are elevating standards of care for patients with both obesity and HF. Retrospective studies of BSx for the primary prevention and secondary treatment of HF are expanding our understanding of the obesity-HF relationship, and a heart failure with preserved ejection fraction (HFpEF)–specific AOM clinical trial confirms the appropriateness of obesity treatment in this population. However, fundamental questions remain regarding the optimal approach to obesity treatment within the HF population, with probable differences in these risk-benefit considerations between the HFrEF and HFpEF populations. This review summarizes currently published data regarding the epidemiology of obesity and HF, opportunities to prevent HF by treating obesity, the rationale and caveats regarding intentional weight loss for patients with HF across the lifestyle, surgical, and medication domains, and particularly the growing role of the AOMs for patients with obesity and HFrEF or HFpEF (Central Illustration).
Central Illustration. Treatment of Obesity Across the Lifestyle, Surgery, and Medication Domains for Primary Prevention and Secondary Treatment of HF
Visual summary of the best available current obesity treatment data from randomized clinical trials or nonrandomized cohort studies informing primary prevention of HF and secondary treatment of HF, further split into the HFpEF vs HFrEF phenotypes where available. Most relevant data from studies n ≥50. Made with BioRender.com. BMI = body mass index; HF = heart failure; HFpEF = heart failure with preserved ejection fraction; HFrEF = heart failure with reduced ejection fraction; NR = nonrandomized; RCT = randomized controlled trial; RYGB = Roux-en-Y gastric bypass; WL = weight loss, placebo-adjusted.
JACC Heart Fail. 2024;12(9) © 2024 American College of Cardiology Foundation