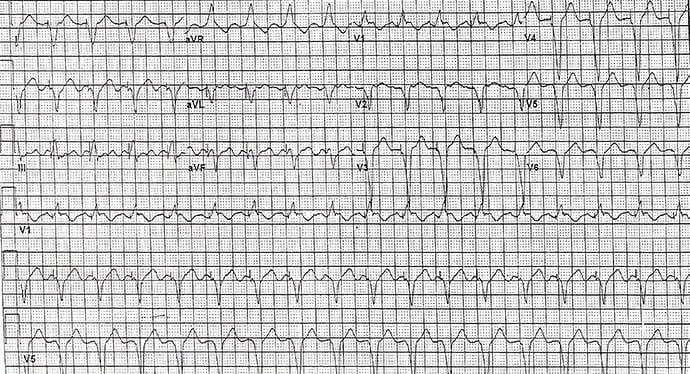
A 76-year-old woman with known ischemic cardiomyopathy, a left ventricular ejection fraction of 25%, and a previously inserted pacemaker presents to her cardiologist concerned that there is a problem with the pacemaker because her heart rate is persistently rapid.
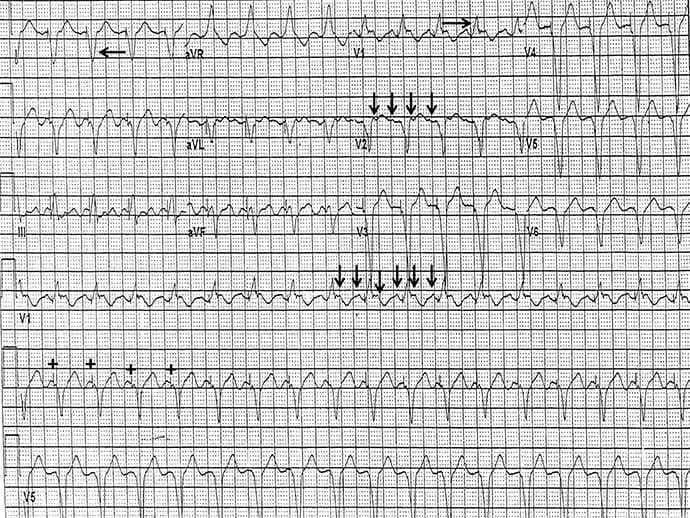
The correct diagnosis is atrial arrhythmia with 2:1 biventricular ventricular pacing (Figure 2).
Discussion
The rhythm is regular at a rate of 114 beats/min. A ventricular pacing stimulus occurs before each QRS complex (+). Prior to the ventricular paced complex there is a P wave; hence the mode of pacing is atrial-sensed ventricular-paced, or P-wave synchronous ventricular pacing.
The QRS complex is wide (0.16 sec) because of ventricular capture from the pacing stimulus. A QS complex occurs in lead I (←), indicating that the ventricular impulse originates from the left side and moves to the right. This is consistent with an initial left ventricular stimulus, ie, biventricular pacing.
Lead I is the only bipolar right-left lead. Any impulse traveling leftward generates a positive deflection (R wave) in lead I; if the impulse moves rightward, the impulse is negative in lead I (ie, initial Q wave or QS complex). With a right ventricular lead, the QRS complex in lead I should be a broad R wave because the impulse is traveling from right to left. The axis is indeterminate between -90° and +/-180° (QRS complex negative in leads I and aVF), which is often seen with a biventricular pacemaker.
Further supporting a biventricular pacemaker is a tall R wave in lead V1 (→), indicating that the impulse is moving toward the right. This is not as useful as the QRS morphology in lead I, because an RV lead at the septum may also give this pattern. In addition, there is a QS pattern in leads V4-V6. However, this may also be seen with a left bundle branch block pattern resulting from right-ventricular pacing. Therefore, the most important lead diagnostic of biventricular pacing is lead I, which is the only bipolar right-left lead.
Organized atrial waveforms are seen (↓) particularly in lead V1-V2. The PP interval is regular at an atrial rate of about 240 beats/min. It is unclear if this is an atrial tachycardia that is fast or atrial flutter that is slow. Nevertheless, based on the post ventricular atrial refractory period, which determines the upper rate limit of the pacemaker (ie, whether atrial activity is sensed by the atrial lead), the pacemaker is only able to sense every other P wave, resulting in a ventricular pacing stimulus in a 2:1 pattern. This is often referred to as a pseudo second-degree atrioventricular block.
Philip Podrid, MD, is an electrophysiologist, a professor of medicine and pharmacology at Boston University School of Medicine, and a lecturer in medicine at Harvard Medical School. Although retired from clinical practice, he continues to teach clinical cardiology and especially ECGs to medical students, house staff, and cardiology fellows at many major teaching hospitals in Massachusetts. In his limited free time he enjoys photography, music, and reading.

