A 3-day-old full-term female infant with no concerning prenatal history was evaluated at her pediatrician’s office for a routine follow-up visit after hospital discharge. Her parents reported a small red lesion on the scalp, present since birth. Concerned about its appearance, the pediatrician submitted a pediatric teledermatology consultation. Upon review of the images, which depicted a violaceous papule with a surrounding ring of hair (Figure 1), an in-person dermatology evaluation was recommended.

At the pediatric dermatology clinic a few days later, physical examination revealed a slightly erythematous macule on the scalp with an associated hair collar. No palpable mass was detected, and the lesion was nonpulsatile. The parents noted that the lesion occasionally appeared more prominent when the infant cried. No additional cutaneous abnormalities were identified.
The patient was born to a G1P1 mother at 41 weeks via an unassisted vaginal delivery. She was exclusively breastfed and thriving per parental report.
The correct diagnosis is sinus pericranii.
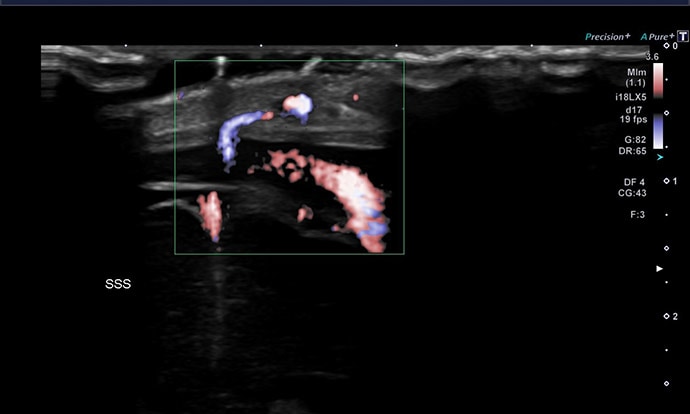
The presence of the hair collar sign prompted further evaluation with cranial ultrasonography (Figure 2), which revealed a small, easily compressible vessel beneath the scalp lesion, demonstrating homogeneous color flow on Doppler imaging. The vessel extended through the skull into the superior sagittal sinus, confirming the diagnosis of sinus pericranii (SP). On the basis of these findings, the patient was referred to neurosurgery for further management.
Discussion
SP is a rare vascular anomaly in which extracranial venous structures communicate with the intracranial venous system via emissary and diploic veins. These lesions typically present as soft, compressible, blue or violaceous papules or nodules that may fluctuate in size with changes in intracranial pressure, such as crying or straining. The lesions may be pulsatile or nonpulsatile and can be associated with alopecia or localized erythema.

SP is most commonly located on the frontal scalp but also has been reported in the occipital, parietal, and temporal regions. While often asymptomatic, some patients may experience headaches, vertigo, or localized pain. Potential complications include bradycardia, bradypnea, hearing loss, hemorrhage, embolism, infection, and ataxia.
SP has been associated with developmental venous anomalies such as persistent primitive falcine sinus, hypoplasia, or malposition of the straight or transverse sinuses, and aneurysmal malformations of the basal vein of Rosenthal or the vein of Galen. It can also be linked to meningocerebral anomalies, including atretic cephalocele, meningeal heterotopia, and corpus callosum aplasia. These associations suggest that SP may serve as an alternative venous drainage pathway in the presence of underlying intracranial developmental anomalies.
The hair collar sign, characterized by a ring of terminal hairs surrounding a scalp lesion, is a clinical marker of cranial dysraphism. A retrospective review by Bessis and colleagues identified associated anomalies such as cranial bone defects with direct communication with the central nervous system, venous malformations, and neuroectodermal abnormalities, with meningeal heterotopia being the most common neuroectodermal association. Although rarely described in the context of SP, its presence in this case underscores the need for neuroimaging to assess potential intracranial involvement.
Given the patient’s age and clinical findings, cranial ultrasonography was performed as an initial imaging modality and confirmed the diagnosis. MRI with contrast is the preferred diagnostic study for SP, however, as it provides a comprehensive evaluation of associated cerebral and vascular anomalies. Bessis and colleagues also noted that cranial and transfontanellar ultrasonography have a high false-negative rate; thus, a negative ultrasound should prompt further evaluation with MRI and MR venography.
This case emphasizes the importance of recognizing the hair collar sign as a potential marker of underlying neurocutaneous anomalies. SP, although rare, should be considered in the differential diagnosis of congenital scalp lesions, particularly those that change with fluctuations in intracranial pressure. MRI remains the gold standard for diagnosis and assessment of associated anomalies. Early recognition and referral to neurosurgery are essential for appropriate management and surveillance of potential complications.

